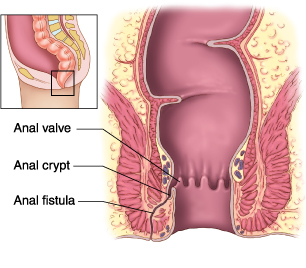
 Anal fistula refers to an infected tunnel that sometimes develops between your skin and your anus, the muscle opening at the end of your digestive tract. You usually experience analfistula because of an infection that develops and starts in an anal gland. The infection may also cause an abscess that drains spontaneously or should be surgically removed. More than half of people who deal with an anal abscess end up developing a fistula. It is, however, not possible to predict when the fistula will develop. If it has already developed, it is important to consult with your doctor and identify a suitable fistula treatment.
Anal fistula refers to an infected tunnel that sometimes develops between your skin and your anus, the muscle opening at the end of your digestive tract. You usually experience analfistula because of an infection that develops and starts in an anal gland. The infection may also cause an abscess that drains spontaneously or should be surgically removed. More than half of people who deal with an anal abscess end up developing a fistula. It is, however, not possible to predict when the fistula will develop. If it has already developed, it is important to consult with your doctor and identify a suitable fistula treatment.
How Do I Know I Have Anal Fistula?
As mentioned already, anal fistulas are the outcome of anal abscesses. You may also end up having an anal fistula if you're suffering from Crohn's disease or other conditions, such as tuberculosis, trauma, diverticulitis and cancer, may cause an anal fistula.
If you have already developed an anal fistula, you may notice certain symptoms, including swelling and pain around your anus, bleeding, recurrent anal abscesses, and pain with bowel movements. You will also notice foul-smelling or bloody drainage from an opening around your anus. The pain may subside after drainage. You may also experience irritation of your skin around the anus, chills, fever and a general feeling of fatigue.
When to Seek Medical Help?
It is important not to ignore the symptoms mentioned above. If you're noticing any drainage or feeling constant, throbbing pain around your anus, it is a good idea to discuss your problem with your doctor who would evaluate the situation to identify the best anal fistula treatment. Your doctor may also refer to a specialist, such as a colorectal surgeon, for proper diagnosis.
How to Diagnose Anal Fistula
Your doctor will examine the area around your anus to diagnose an anal fistula. They will look for an external opening around your anus. If they find one, they will use specific ways to determine its direction and depth. Sometimes, a fistula is not visible on your skin, but your symptoms will help your doctor know that you have already developed an anal fistula. They may start with anoscopy, using a special instrument to see inside your rectum and anus. They may also ask for an ultrasound or MRI to define the fistula tract.
After your physician has diagnosed an anal fistula, the next step would be to order some more tests to rule out the possibility of developing Crohn's disease. This is because more than 25% of people with Crohn's disease will develop anal fistulas. Your doctor will take x-rays, blood tests, etc., to make a decision.
How to Deal With Anal Fistula
It is important to discuss your treatment options with your doctor after you have been diagnosed with anal fistula. They will determine the best anal fistula treatment in your situation. It usually starts with specific changes made to your diet. A proper anal fistula diet usually helps a lot in improving your condition.
You may, however, need to use medical treatments to deal with complex situations. These treatment options will help repair anal fistula and prevent recurrence. They also can protect your sphincter muscles and prevent fecal incontinence. Here are some of the most common fistula treatment options:
- Fistulotomy: The procedure involves cutting the internal opening of the fistula to flush out the infected tissue. The surgeon will flatten the channel after flushing out and stitch it. The surgeon may decide to remove some of the channel in case a fistula is more complicated in nature. Your surgeon will divide the procedure in two stages if they cannot find the entire channel or they have to cut a bit of sphincter muscle.
- Advancement Rectal Flap: Your surgeon will create a flap from the rectal wall before they remove the fistula. Then they use the flap to cover the repair. The best thing about this treatment is that the surgeon doesn't have to cut much of the sphincter muscle.
- Seton Placement: The procedure involves placing a latex or silk string into the fistula to drain the infection.
- Fibrin Glue and Collagen Plug: The procedure starts with clearing the channel. Then surgeon will stitch it to close the opening and inject special glue made from fibrin into the tract. They will then seal it with a plug of collagen protein.
- Ligation of the Intersphincteric Fistula Tract (LIFT): You may have to opt for this two-stage treatment for your deep or more-complex fistula. The procedure lets your surgeon to access the fistula between your sphincter muscles, so there is no need to cut the sphincter muscles. In the first step, your surgeon will place a seton into the tract that will widen over time. The next stage will involve removing all infected tissues and closing the opening.
- Treatment for Complex Fistula: You will need a more invasive procedure for a complex anal fistula. Ostomy and stoma is one good choice that involves creating a temporary opening in your abdomen to direct waste into a specially made bag. Muscle flap is another option that involves filling the channel with healthy muscle tissue from your labia, thigh or buttocks.
- Follow-Up Care: Whatever the treatment option is, it is important to follow up with your doctor after your surgery. It is important to soak the affected area in warm water or take warm showers to accelerate healing. You may also have to be on laxatives or stool softeners for some time to prevent complications.